Medication Disruptions
My Role: UX Researcher | feb 2023
Overview
OptumRx portal wanted to uncover new ways to help customers to solve medication disruptions. The design team developed two prototypes one which they knew could be produced today and the other was an ideal state. Depending on the results of the research, leadership would look to get buy in to create the ideal state and start understanding what it would take to create it.
Terms to know
Disruptions = when a prescription medication is no longer covered, needs prior authorization from a doctor or an alternate medication needs to be choose
(n=#) = sample symbol for the number of participants of the full user group that represent the finding
THings to keep in Mind
No client data is being shown in any of the images below
Research Goals
Understand if the content and steps are clear on the medication details page while solving a medication disruption
Discover if the options (share with prescriber, schedule a call with Optum RX, and select replacement medication) provided on Medication Details page meet participant expectations and next actions are clear
Understand overall feelings of Optum proactively reaching out to the prescriber to solve a disruption
Gather first impressions of an at-home genetic test to better match with an alternative or replacement medication
Methodology & Participants
Research METHODOLOGY
7 one-hour usability sessions via Teams + 1 pilot participant
All participants were recruited from a third party vendor and identified as having a disruption in their medication within the past year
Two prototypes were tested in randomized order per participant:
Choices Flow (option that can be implemented today)
Automatic Flow (option that would need further discovery if it could get produced)
Two UX metrics questions were asked per site to gauge confidence and satisfaction with the options listed in each prototype
Participant background
Found out their medication was no longer covered at the pharmacy while going to pick up their meds (n=6)
Situation created frustration and distrust in the insurance company due to the lack of transparency as to why their medication was no longer covered (n=2)
Angry and desperate to understand what comes next, thinking they will have to start all over again to find a medication that works for them (n=3)
Concerned they will have to be off their medication for a number of days until this gets resolved (n=2)
Reluctantly accepted their medication will no longer be covered but wanted advanced notice in order to take steps to make sure they have medication (n=5)
Top Themes
Disruptions in a user’s medication can be an emotionally triggering experience which can have long lasting affects and resurface while interacting with designs and content
There is a desire for more information about how listed replacement medications compare to the original medication
Optum proactively reaching out to the provider caused feelings of relief and confidence that their medication disruption would be taken care of
Reassurance and supporting data from Optum will be needed in order for users to feel comfortable with at home genetic testing
Flow A: Choices Flow
Home Screen
Immediately notices their medication is no longer covered (n=6)
After clicking expected to see an explanation as to why their medication is no longer covered (n=5)
Alert
Alternating views if the alert content was helpful or not
Expect clicking on learn more would give an explanation as to why their medication is no longer covered (n=3)
Found the information generic and not personalized (n=4) and require them to call Optum for an explanation (n=2)
Satisfied with the given explanation in learn more (n=3) and noticed the next steps and was appreciative that action items were given (n=3)
Share with your prescriber tile
Would download the list and share it with their doctor at their appointment (n=4)
Trusted in Optum's list of replacement medication (n=3)
Look at the download list as an opportunity to do their own research prior to talking to their prescriber (n=2)
Reasons to send a message was because they were familiar with this type of interaction with their provider (n=2) or to save time (n=1)
Schedule a Call
Would not choose to schedule a call (n=5)
Overall concerned about the wait time if they were to call (n=2)
Feel more comfortable talking to their doctor (n=3)
Wasn't sure what information they would receive or what Optum could do for them if
they called (n=4)Reasons they would call:
Get more information about why their medication is no longer covered (n=2)
Issue with the site (n=2)
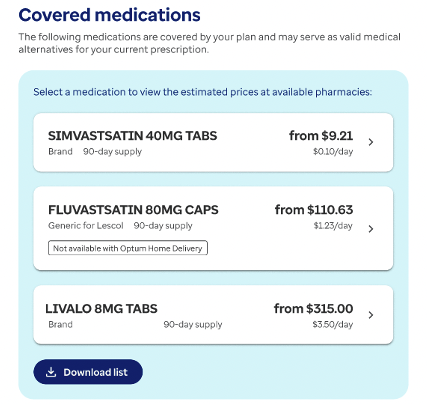
Select replacement medication
Having the prices shown was valuable because participants could see what was closest to what they are paying now (n=5)
Expecting more detail in this section and to show a comparison to their current medication (n=4)
Wouldn't choose a replacement for themselves in this section, wanted to call their prescriber (n=5)
After calling the doctor would utilize this section to choose a replacement medication (n=2)
If desperate would choose a medication to make sure they don’t run out (n=1) or if they could only afford one of the options (n=1)
Satisfaction Score
Overall, how satisfied are you with the options presented on how to solve your medication no longer being covered?
Average Score 5.4 out of 7
Reasoning for a score of 6 or 7
Satisfied with the screens because it provided actions to solve their medication no longer being covered (n=5)
Reasoning for a score of 2 or 3
Unsatisfied because they were not comfortable with the select replacement medication option being on the screen (n=2)
Wanted to see a comparison between the medication (n=1) explanation of why the change occurred (n=1)
Confidence Score
Overall, how confident are you that you would be able to solve the issue of your medication no longer be covered?
Average Score 6.1 out of 7
Reasoning for a score of 6 or 7
Confident because there is lot of options to choose from and provides lots of information (n=5)
Would like to see more information about when the medication will no longer be covered so they can take the necessary steps to prepare (n=2)
Flow B: Automatic Flow
Homepage
Having the date was helpful because it gave time to resolve the issue prior to it being no longer covered (n=7)
Felt the banner was a notification, their first instincts were not to click on it to resolved the issue (n=4)
Alert
Wanted to get more information as to why their medication is no longer covered would read the content and would be their first step (n=3)
Alternating views if the alert content was helpful or not
Feels like it is not descriptive or providing information as to why their prescriptions isn't covered (n=2)
Satisfied with the reasoning provided (n=2)
Optum Reached Out
Understood the content was telling them Optum reached out to their provider (n=7)
Felt relief and confidence that Optum would take care of the disruption on their behalf (n=7)
Liked this option because they expected the disruption to be solved quicker then doing it themselves (n=5)
Would call their doctor to check in depending how long it has been since Optum reached out to their doctor (n=3)
Expected Optum to automatically reach out on the customers behalf (n=6)
Doctor Got Back
Remarked they were comfortable that it was their prescriber who has chosen the alternative (n=3)
Wanted to see how similar or different the two medications were (n=3)
Reasons to not click approve would be if the new medication was different type such as a pill to injectable (n=2)
With such a low-price difference would want to reach out to their doctor if they could stay on their original medication (n=3)
Satisfaction Score
Overall, how satisfied are you with the option presented on how to solve your medication no longer being covered?
Average Score 6.6 out of 7
Reasoning for a score of 6 or 7
Satisfied because they know Optum is doing all the work for them and do not have to worry (n=5)
Reasoning for a score of 5
Unsatisfied with the explanation as to why the medication is being disrupted and how the new medication is an equivalent (n=1)
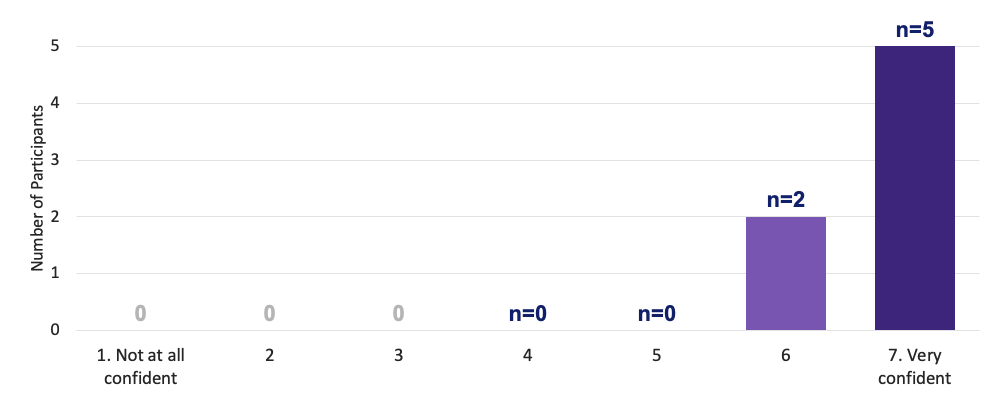
Confidence Score
Overall, how confident are you that you would be able to solve the issue of your medication no longer be covered?
Average Score 6.7 out of 7
Reasoning for a score of 6 or 7
Instills confidence because their provider is involved in the process of choosing a new medication (n=4)
Confident because they know it is going to be resolved (n=2)
Recommendations
Choices Flow
When possible, notify members as soon as possible their medication is being disrupted
Update content in schedule a call with Optum RX tile to inform users what to expect if they were to call and how Optum can help
Brainstorm ideas how select replacement medication could provide more information to users
Features such as compare between the covered medication and the original no longer covered medication can provide the user with more information
Automatic Flow
Provide clarity on how they will be notified once their prescriber has chosen a replacement medication
Update heading to be transparent about if users need to opt-in
Self-service option to cancel prescription request
Comparison between the covered replacement and medication no longer covered
Self-service option to reject covered replacement